JODH SINGH NAHAL
age 16
Canada-Wide Science Fair: Bronze Medal Excellence Award and Western University Scholarship | Sanofi Biogenius Provincial Awards: Genome BC Scholarship Award | Cariboo Mainline Regional Science Fair: Best Senior Project, Gold Medal, and Thompson Rivers University Scholarship
Edited by Mehar Gill
INTRODUCTION
Globally, around 80% of older adults have at least one chronic disease (National Council on Aging, 2021). According to WHO (2019), diabetes mellitus or diabetes is a global epidemic affecting 422 million people worldwide. It is one of the leading causes of death in the world, with 4.2 million deaths in 2019 alone. According to most physicians, type-2 diabetes mellitus (T2DM) is a progressive, life-long disease, while at the same time there is a consensus that it is a metabolic disorder, and diet and lifestyle changes play a significant role in managing T2DM. It could reduce the risk of diabetes by 30-67% (Maghsoudi & Azadbakht, 2012). It has been known since 1930 that T2DM can be reversed with a whole-food plant-based (WFPB) diet (Rabinowitch, 1935), but unfortunately there is hardly any awareness about it.
This case study was started during the start of the COVID-19 pandemic, which in particular made immunocompromised people nervous. The case study participant, N.N., had T2DM and other chronic conditions; she had a family history. N.N.’s parents and grandparents have chronic diseases; her grandmother died of uncontrolled diabetes complications. Thus, N.N. was motivated to stay healthy. It was a 1-year longitudinal and experimental case study about N.N: a 46-year-old overweight female with low energy and fatigue, and on multiple prescription medications for chronic diseases.
On the basis of extensive research, it was found that low-carb high-fat (LCHF) diets only have short-term health improvements and treat only the symptom of diabetes (high blood glucose) but not the disease, rather it makes the disease much worse because the disease is carbohydrate intolerance, and eating low-carb worsens carbohydrate intolerance. That is why WFPB diets do better in glucose tolerance tests than LCHF diets (Sweeny, 1927). Also, insulin resistance is not caused by carbohydrates, but by the storage of fat in tissues that are meant to store glucose, such as in kidneys, liver, heart, and skeletal muscle. This is lipotoxicity. When intramyocellular lipids (fat inside the muscle cells, especially the trans-fat and saturated fat) builds up, the insulin is not able to allow glucose to get into the cells, causing insulin resistance and beta-cell dysfunction (DeFronzo, 2010), and the glucose stays in the blood causing hyperglycemia. This was not known until MRI was used to see what was happening inside the muscle cells (Greger, 2016). Moreover, cardiovascular disease (CVD) accounts for 65% of all diabetes-related deaths, and LCHF diet causes CVD.
The main goal of this project was to lower HbA1c and reverse type-2 diabetes. Thereby, this study aims to investigate if it is possible to reverse chronic T2DM with diet and lifestyle modifications; and to find the effects of WFPB diet, exercise, time-restricted eating, and losing extra weight, on the blood glucose level and other health markers. To investigate this, extensive online research and meta-analysis reviews were conducted. Moreover, three comprehensive experiments, more than 200 blood glucose tests and lab tests were also conducted, along with many statistical tests.
METHODS
On the basis of extensive meta-analysis reviews, an evidence-based WFPB diet was selected for N.N. (Chen, Z. et al., 2018; Coote & Sadeghi, 2017; Maghsoudi & Azadbakht, 2012; Mayo Clinic, 2020, 2022; McMacken & Shah, 2017; Physicians Committee for Responsible Medicine, n.d.; Qian et al., 2019; Reynolds et al., 2020; Smithson, 2019; Tello, 2018; Toumpanakis, 2018; Tuso et al., 2013; Vieira, 2019; WebMD, 2021a; Wiginton, 2021; Yokoyama et al., 2014). Research shows that around 10% weight loss can reverse T2DM (Anderson et al., 2003; Chen Y. et al., 2018; Franz, 2007; Franz et al., 2015; Laguipo, 2019; Leontis, 2018; Maula et al., 2020; Sheehan, 2020; WebMD, 2021b), and time-restricted eating and exercise also has a major effect on the blood glucose levels (Colberg et al., 2016; University of Adelaide- ScienceDaily, 2019). Fiber reduces insulin resistance (Mayo Clinic, 2022) and is found only in plants; it also lowers the risk of heart disease (Diabète Québec, 2014; Fletcher, 2019; Grains & Legumes Nutrition Council, n.d.; Jenkins et al., 2012; McRae, 2018; Polak et al., 2015; Post et al., 2012; Roland, 2020; Schulze et al., 2007; Sievenpiper et al., 2009; Threapleton et al., 2013; Times of India, 2020). Also, binge eating on a regular basis may disturb your glucose metabolism (Fritz, 2018). All the safety precautions were taken, and N.N. switched from a partially unhealthy vegetarian diet to a completely healthy vegetarian diet (WFPB diet), and also exercised regularly and did time-restricted eating, as shown in Table 1 below.
To lower HbA1c and reverse T2DM – the main goal of this study, three comprehensive experiments were conducted. Experiment #1 was conducted to control the post-meal blood glucose spikes; it investigated the effects of four physical activities: sitting (the control group), walking~ 5-6 km/h, moderately going up-down stairs, and interval training (IT), on 2-hours post-meal blood glucose levels, and to see if there is any statistically significant correlation between them. Experiment #2 was conducted to control morning’s fasting blood glucose spikes; it tested the effects of two dinner timings: ½-hour before bed and 3-hours before bed, on next morning’s fasting blood glucose levels, and to find if the result is statistically significant. Finally, Experiment #3 was conducted to test the effects of a switch from a partially unhealthy vegetarian diet to a completely healthy vegetarian diet (WFPB diet), and more regular physical activity, on lowering HbA1c and reversing type-2 diabetes. N.N.’s blood test was performed every three months at the medical laboratory for a year, followed by an appointment with her family doctor each time.
RESULTS
In Experiment #1 (Figure 1 below), it was found that instead of just ‘sitting’ (control), 30 minutes of any kind of these physical activities, 1.5 hours after meal, were 2.4 to 4.1 times more effective in controlling 2-hours post-meal blood glucose spikes. From Anova: Single Factor statistical test, it was found that there was a statistically significant difference between the four groups (F(3,12) = 5.6 > F-critical = 3.5, and P-value = 0.013 < α = 0.05). Tukey HSD statistical test confirmed that the ‘sitting’ (control) was the only group that was statistically significantly different from each of the other three groups – walking, stairs, and IT, with P-values <0.05, <0.01, and <0.01, respectively. Through Correlation and Regression statistical tests, a strong and highly statistically-significant negative-correlation was found between the levels of physical activities and the rise in the blood glucose levels. The Pearson’s correlation coefficient, r = -0.73, and the p-value = 0.0013 < α = 0.01. Moreover, when an outlier, trial #2 (very less food consumption), was excluded, the correlation was even stronger, r = -0.95, and even more statistically significant with a very small p-value = 2.95E-06.
In Experiment #2 (Figure 2 below), it was found that if dinner is finished around 3-hours before bed instead of just before bed, it is more than twice as effective in controlling next morning’s fasting blood glucose level. T-Test: Paired Two Sample for Means confirmed that both the groups were statistically significantly different from each other (t(3) = 3.4 > t-critical = 3.2, p-value = 0.043 < α = 0.05).
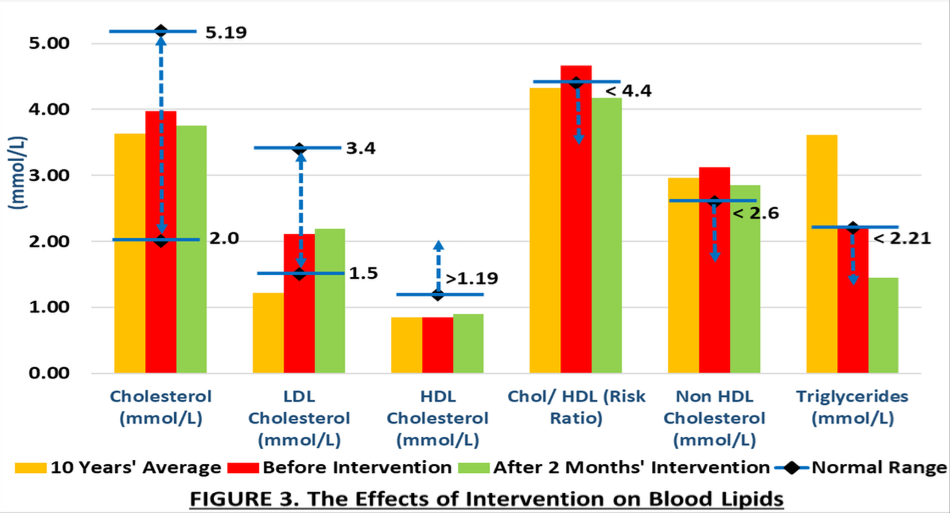
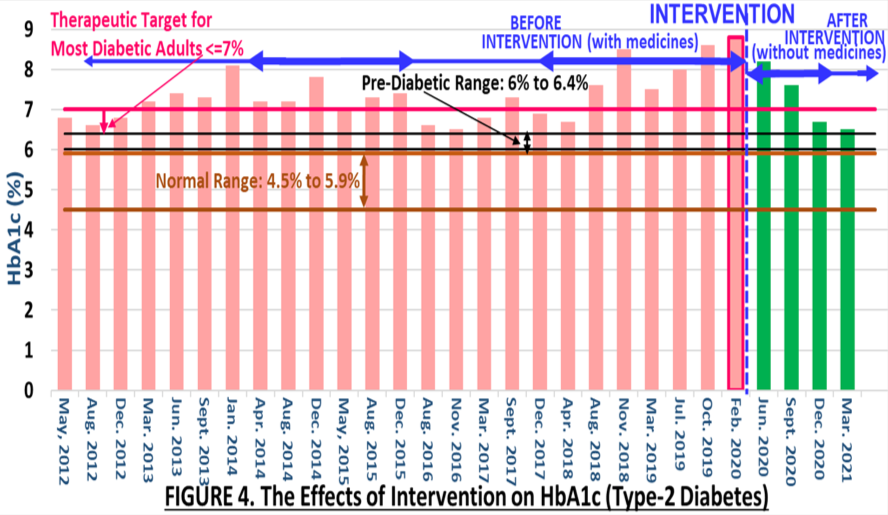
In Experiment #3, it was found that: Weight and BMI: N.N.’s body weight dropped consistently from 150 to 125 lbs. She lost 25 lbs, which is 16.7% of the body weight. Her BMI dropped from 26.6 (overweight range) to 22.1 (normal weight range). Hypothyroidism: The Synthroid medication that N.N. used to take for the past eight years, was reduced from 125 to 100 mcg. Blood Lipids (Figure 3 below): N.N.’s cholesterol level dropped and got better. Her HDL cholesterol increased slightly. Although, the LDL increased slightly, but it was still in the safe normal range. The risk-ratio dropped from 4.67 to 4.17 (normal range) and the non-HDL cholesterol dropped from 3.12 to 2.85 mmol/L. Moreover, the triglycerides that was always very high (10 years’ average=3.6), dropped to 1.45 mmol/L (safe normal range) – the lowest ever in 10 years. Hypertension: N.N.’s blood pressure dropped from a high 142/ 89 mmHg to a normal 126/ 78 mmHg range; and the Ramipril 10 mg medication that N.N. used to take for the past three years was stopped. HbA1c (Figure 4 below): There were four consecutive sharp declines in N.N.’s HbA1c after intervention (without any medicines) that never happened in the past nine years even with 2000mg Metformin/day. N.N.’s HbA1c that was very high at 8.8%, almost dropped into the pre-diabetes range. Her HbA1c dropped to 6.5% which was one of the lowest in the past 10 years; it was not only lower than before-intervention HbA1c of 8.8%, but was also lower than its nine years' average of 7.4%. She went from 2000 mg of Metformin/day to none.
DISCUSSION
Through experimental investigations, it was found that dietary and lifestyle modifications can reverse even 10 years’ chronic diseases. As a result of interventions, N.N. not only lost 25-pounds and normalized her BMI, but she also reversed her 10-year chronic T2DM, 3-year chronic hypertension, and stopped all medications. Moreover, she also significantly improved her 8-year chronic hypothyroidism and her lipids profile as well. Therefore, N.N.’s chances of getting a heart attack, stroke, limb amputations, kidney, nerve, and eye damage, significantly decreased. Because of interventions, N.N. took 1,825 less prescription medicine tablets in a year, so she saved herself from various medicinal side-effects. N.N. felt more energy and strength; she was able to enjoy even mountain biking that never happened before. It was found that what medicinal treatments could not achieve in nine long years, WFPB diet and exercise achieved in just under one year without any drugs. Although, the positive changes started showing in just two months of full intervention.
CONCLUSION
It is possible to reverse even chronic diseases with dietary and lifestyle changes. WFPB diet works, besides so many health benefits, it is also good for the environment, stops animal cruelty, and eliminates most viral and bacterial infections—so it is kind of a one-diet-fix-all diseases and issues. N.N.’s family doctor was very pleased with N.N.’s blood-work report and asked her to continue what she was doing for her health. The results were not temporary, but were rather stable and consistent. This study’s outcomes unfortunately didn’t come from the established medical system, but from the extensive research-and-application of the evidence-based data. It is hoped that other people get inspired by this study’s results and know that it is possible to reverse not only a newly diagnosed, but even a decade long chronic diseases, and thereby, like N.N., one can significantly reduce their chances of getting a heart attack, stroke, limb amputations, kidney, nerve and eye damage etc., and live a stress-free life.
WORKS CITED
Anderson, J. W., Kendall, C. W., & Jenkins, D. J. (2003). Importance of weight management in type 2 diabetes: Review with meta-analysis of clinical studies. Journal of the American College of Nutrition, 22(5), 331–339. https://doi.org/10.1080/07315724.2003.10719316
Chen, Y., Yang, X., Wang, J., Li, Y., Ying, D., & Yuan, H. (2018). Weight loss increases all-cause mortality in overweight or obese patients with diabetes: A Meta-analysis. Medicine 97(35), p e12075. http://DOI.org/10.1097/MD.0000000000012075
Chen, Z., Zuurmond, M.G., van der Schaft, N. et al. (2018). Plant versus animal-based diets and insulin resistance, prediabetes and type 2 diabetes: the Rotterdam study. Eur J Epidemiol 33, 883–893. https://doi.org/10.1007/s10654-018-0414-8
Colberg, S. R., et al. (2016). Physical activity/exercise and diabetes: A Position statement of the American Diabetes Association. Diabetes Care, 39(11): 2065–2079. https://doi.org/10.2337/dc16-1728
Coote, S., & Sadeghi, A. (2017). Diabetes - cause, prevention, treatment and reversal with a plant-based diet. Rise of the vegan. www.riseofthevegan.com/blog/diabetes-reversal-with-plant-based-diet.
DeFronzo R. A. (2010). Insulin resistance, lipotoxicity, type 2 diabetes and atherosclerosis: the missing links. The Claude Bernard Lecture 2009. Diabetologia, 53(7), 1270–1287. https://doi.org/10.1007/s00125-010-1684-1.
Legumes and Pulses. (2014). Diabète Québec. www.diabete.qc.ca/en/living-with-diabetes/diet/food-and-nutrients/legumes-and-pulses/.
Fletcher, J. (2019). Are beans good for diabetes? Medical News Today. www.medicalnewstoday.com/articles/325001.
Franz, M. J. (2007). The Dilemma of weight loss in diabetes. Diabetes Spectrum, 20 (3): 133–136. https://doi.org/10.2337/diaspect.20.3.133
Franz, M. J., Boucher, J. L., Rutten-Ramos, S., & VanWormer, J. J. (2015). Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: A Systematic review and meta-analysis of randomized clinical trials. Journal of the Academy of Nutrition and Dietetics, 115(9), 1447–1463. https://doi.org/10.1016/j.jand.2015.02.031
Fritz, A. (2018). 5 very real dangers of binge eating. Keck Medicine of USC. https://keckmedicine.org/blog/5-very-real-dangers-of-binge-eating/
Legumes and Diabetes. (n.d). Grains & Legumes Nutrition Council. www.glnc.org.au/legumes-2/legumes-and-health/legumes-and-diabetes/.
Greger M. (2016). Fat is the cause of type 2 diabetes. NutritionFacts.org. www.nutritionfacts.org/2016/11/17/fat-is-the-cause-of-type-2-diabetes/.
Jenkins, D., Kendall, C., Augustin, L., et al. (2012). Effect of legumes as part of a low glycemic index diet on glycemic control and cardiovascular risk factors in type 2 diabetes mellitus: A randomized controlled trial. Arch Intern Med. 2012;172(21):1653–1660. http://doi.org/10.1001/2013.jamainternmed.70
Laguipo, A. B. B. (2019). Weight loss is the key in battling type 2 diabetes, study reveals. News Medical Life Sciences. www.news-medical.net/news/20190930/Weight-loss-is-the-key-in-battling-type-2-diabetes-study-reveals.aspx
Leontis, L. M. (2018). Type 2 diabetes: Tips to lose weight successfully. EndocrineWeb. www.endocrineweb.com/conditions/type-2-diabetes/type-2-diabetes-how-lose-weight
Maghsoudi, Z., & Azadbakht, L. (2012). How dietary patterns could have a role in prevention, progression, or management of diabetes mellitus? Review on the current evidence. Journal of research in medical sciences: The official journal of Isfahan University of Medical Sciences, 17(7), 694–709. www.ncbi.nlm.nih.gov/pmc/articles/PMC3685790/.
Maula, A., Kai, J., Woolley, A. K., Weng, S., Dhalwani, N., Griffiths, F. E., Khunti, K., & Kendrick, D. (2020). Educational weight loss interventions in obese and overweight adults with type 2 diabetes: A Systematic review and meta-analysis of randomized controlled trials. Diabetic Medicine: A Journal of the British Diabetic Association, 37(4), 623–635. https://doi.org/10.1111/dme.14193
Type 2 diabetes. (2020). Mayo Clinic. www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193.
Dietary fiber: Essential for a healthy diet. (2022). Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983
McMacken, M., & Shah, S. (2017). A plant-based diet for the prevention and treatment of type 2 diabetes. Journal of geriatric cardiology: JGC, 14(5), 342–354. www.ncbi.nlm.nih.gov/pmc/articles/PMC5466941/#:~:text=Plant-based-diets
McRae, M. P. (2018). Dietary fiber intake and type 2 diabetes mellitus: An Umbrella review of meta-analyses. Journal of Chiropractic Medicine, 17(1), 44–53. https://doi.org/10.1016/j.jcm.2017.11.002
Get the facts on chronic disease self-management. (2021). National Council on aging. www.ncoa.org/news/resources-for-reporters/get-the-facts/chronic-disease-facts/.
Diabetes. (n.d.). Physicians Committee for Responsible Medicine. www.pcrm.org/health-topics/diabetes.
Polak, R., Phillips, E. M., & Campbell, A. (2015). Legumes: Health benefits and culinary approaches to increase intake. Clinical Diabetes; 33 (4): 198–205. https://doi.org/10.2337/diaclin.33.4.198
Post, R. E., Mainous, A. G., King, D. E., & Simpson, K. N. (2012). Dietary fiber for the treatment of type 2 diabetes mellitus: A Meta-analysis. The Journal of the American Board of Family Medicine, 25(1) 16-23; http://DOI.org/10.3122/jabfm.2012.01.110148
Qian, F., Liu, G., Hu, F. B., Bhupathiraju, S. N., & Sun, Q. (2019). Association between plant-based dietary patterns and risk of type 2 diabetes: A Systematic review and meta-analysis. JAMA Intern Med, 179(10):1335–1344. http://doi.org/10.1001/jamainternmed.2019.2195
Rabinowitch I. M. (1935). Effects of the High Carbohydrate-Low Calorie Diet Upon Carbohydrate Tolerance in Diabetes Mellitus. Canadian Medical Association journal, 33(2), 136–144. www.pubmed.ncbi.nlm.nih.gov/20319961/.
Reynolds, A. N., Akerman, A. P., & Mann, J. (2020). Dietary fibre and whole grains in diabetes management: Systematic review and meta-analyses. PLoS Med 17(3): e1003053. https://doi.org/10.1371/journal.pmed.1003053
Roland, J. (2020). What you should know about diabetes and beans. Healthline. www.healthline.com/health/diabetes/beans#takeaway.
Schulze, M. B., Schulz, M., Heidemann, C., Schienkiewitz, A., Hoffmann, K., & Boeing, H. (2007). Fiber and magnesium intake and incidence of type 2 diabetes: A prospective study and meta-analysis. Arch Intern Med. 2007;167(9):956–965. http://doi.org/10.1001/archinte.167.9.956
Sheehan, J. (2020). 8 steps for weight loss success if you have type 2 diabetes. Everyday Health. www.everydayhealth.com/type-2-diabetes/diet/secrets-of-weight-control/.
Sievenpiper, J. L., Kendall, C. W. C., Esfahani, A. et al. (2009). Effect of non-oil-seed pulses on glycaemic control: A systematic review and meta-analysis of randomised controlled experimental trials in people with and without diabetes. Diabetologia 52, 1479-1495. https://doi.org/10.1007/s00125-009-1395-7
Smithson, T. (2019). Can eating more plant-based foods help manage diabetes? U.S. News. https://health.usnews.com/health-news/blogs/eat-run/articles/can-eating-more-plant-based-foods-help-manage-diabetes.
Sweeny J. S. (1927). Dietary factors that influence the dextrose tolerance test: A preliminary study. Arch Intern Med (Chic), 40(6):818–830, https://doi.org/10.1001/archinte.1927.00130120077005.
Tello, M. (2018). Eat more plants, fewer animals. Harvard Health Publishing. www.health.harvard.edu/blog/eat-more-plants-fewer-animals-2018112915198.
Threapleton, D., Greenwood, D., Evans, C., Cleghorn, C., Nykjaer, C., Woodhead, C., & Burley, V. (2013). Dietary fibre intake and diabetes risk: A systematic review and meta-analysis of prospective studies. Proceedings of the Nutrition Society, 72(OCE4), E253. http://doi.org/10.1017/S0029665113002784
These are the healthiest legumes diabetics should include in their diet. (2020). Times of India. www.timesofindia.indiatimes.com/life-style/health-fitness/diet/these-are-the-healthiest-legumes-diabetics-should-include-in-their-diet/photostory/75446527.cms.
Toumpanakis, A., Turnbull, T., & Alba-Barba, I. (2018). Effectiveness of plant-based diets in promoting well-being in the management of type 2 diabetes: A Systematic review. BMJ Open Diabetes Research and Care, 6:e000534. http://doi.org/10.1136/bmjdrc-2018-000534
Tuso, P. J., Ismail, M. H., Ha, B. P., & Bartolotto, C. (2013). Nutritional update for physicians: Plant-based diets. The Permanente Journal, 17(2), 61–66. https://doi.org/10.7812/TPP/12-085
University of Adelaide. (2019). Time-restricted eating shows benefits for blood glucose. ScienceDaily. www.sciencedaily.com/releases/2019/04/190424153634.htm
Vieira, G. (2019). A plant-based diet can reduce your risk for type 2 diabetes, if you do it correctly. Healthline. www.healthline.com/health-news/the-right-plant-based-diet-can-lower-your-risk-for-type-2-diabetes.
Understanding diabetes – diagnosis and treatment. (2021a). WebMD. www.webmd.com/diabetes/news/20190725/plant-based-diet-helps-keep-diabetes-at-bay.
Diabetes basics. (2021b). WebMD. www.webmd.com/diabetes/features/diabetes-weight-loss-diet-plan.
Wiginton, K. (2021). Vegan diet for people who have diabetes. WebMD. www.webmd.com/diabetes/veganism-for-people-who-have-diabetes.
Diabetes. (2019). World Health Organization. www.who.int/health-topics/diabetes#tab=tab_1.
Yokoyama, Y., Barnard, N. D., Levin, S. M., & Watanabe, M. (2014). Vegetarian diets and glycemic control in diabetes: A Systematic review and meta-analysis. Cardiovascular diagnosis and therapy, 4(5), 373–382. https://doi.org/10.3978/j.issn.2223-3652.2014.10.04
ABOUT THE AUTHOR
Jodh Singh Nahal
Currently, I’m pursuing biomedical engineering at UBC Vancouver after winning the Presidential Scholars Major Entrance Scholarship Award; I also won around a dozen other scholarships. I’ve had a strong passion for STEM and sports from my early childhood–played multiple sports throughout my school life, and have won more than 50 regional and national-level STEM awards including six awards and four scholarships at the renowned CWSF–I was selected every year from grade 7-12. This was my grade 11 project; I would like to update that the case-study participant, who later started taking wheat and sugar moderately, is still doing great after 2-years.